Pelvic Organ Prolapse: The Basics.
First, let’s talk about what pelvic organ prolapse is. Essentially, pelvic organ prolapse refers to the descent of one or more of your pelvic organs down into the vagina or in the case of rectal prolapse, the anus. The most common types of prolapse are bladder (cystocele), Uterus (Uterocele) and Rectum (rectocele or rectal prolapse).
Most women have never heard the term pelvic organ prolapse, until they are diagnosed with one. But it is actually very common. Research shows that 50% of women who have had children have some degree of symptomatic or asymptomatic loss of pelvic organ support, resulting in prolapse (Hagen & Stark, 2011) (Diane Lee, 2018).
This is how your pelvic organs look when they are supported.
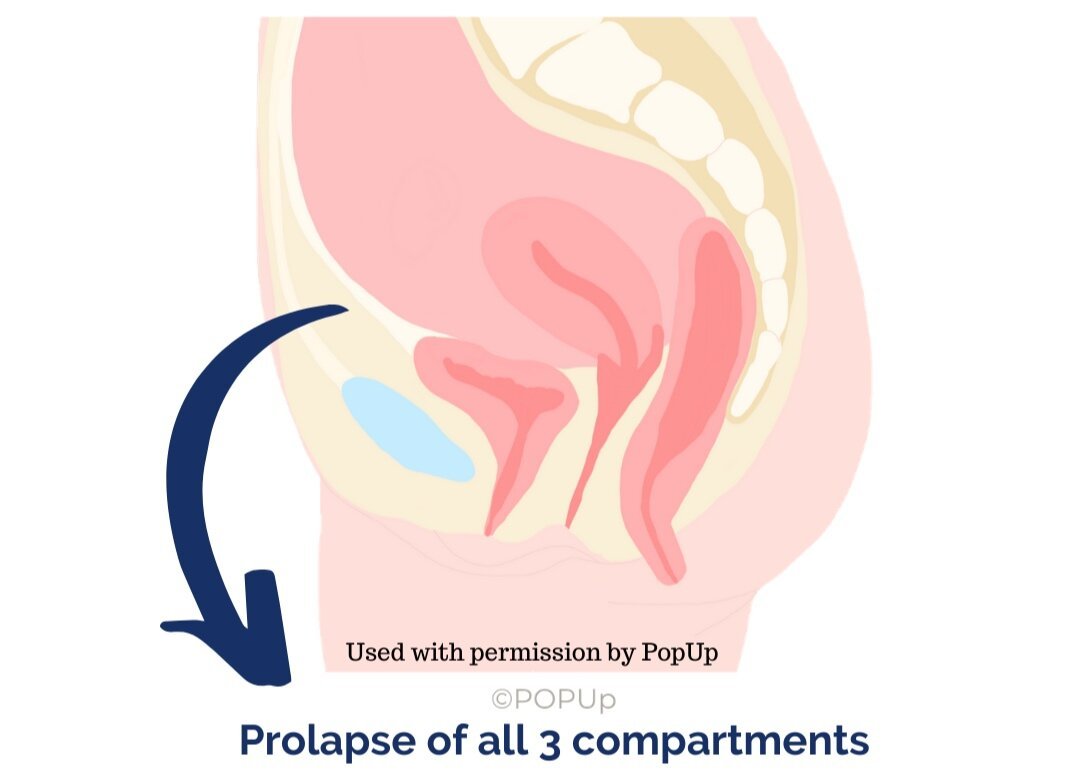
This is how your pelvic organs look when they are prolapsed.
So, What are some symptoms of prolapse?
Symptoms of Pelvic Organ Prolapse
Feelings of heaviness or pressure
Feelings of dragging or bulging
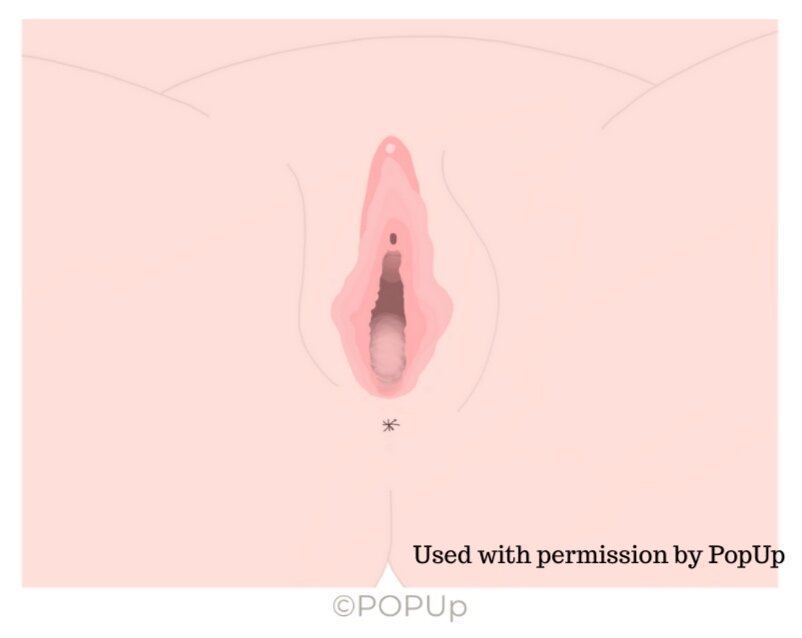
A bulge in the vagina that you can touch or see
Vaginal laxity or looseness
Straining to Empty Bowel Or Bladder
Urinary incontinence (often associated)
Painful intercourse (often associated)
Many women with prolapse will have one or more of these symptoms. However, in some cases women may not feel any symptoms at all. Typically women with prolapse will find that their symptoms are better in the morning or with rest and worse with activity and by the end of the day.
Are Some Women More Likely to Develop a Prolapse?
Some women may be more at risk of developing pelvic organ prolapse. See below
Risk Factors for Prolapse:
Body Mass Index >25
Increasing age
Chronic constipation and or straining
Respiratory issues such as asthma and chronic cough
Family history of prolapse
Vaginal delivery
Heavy lifting and physically demanding occupations
Use of forceps during birth
Levator Ani Avulsion (tearing of the pelvic floor muscles)
“Vaginal Delivery increases the risk of developing a prolapse. One delivery increases the risk by 4. Two or more deliveries increases the risk by 8.4.”
— (Mant et al 1997) (Diane Lee, 2018).
Types of Pelvic Organ Prolapse
Okay, now that we know the risk factors and the symptoms to look for, let’s talk about the different types of prolapse.
Bladder Prolapse (Cystocele)
Occurs when the bladder pushes against the front wall of the vagina towards the vaginal opening.
Uterine Prolapse (Uterocele)
Occurs when the Uterus or Cervix descends down toward the vaginal opening.
Rectocele
Occurs due to weakness in the back wall of the vagina, causing the back wall to push forward towards the vaginal opening.
It is not uncommon for some women to experience more than one type of prolapse.
How Bad Is It?
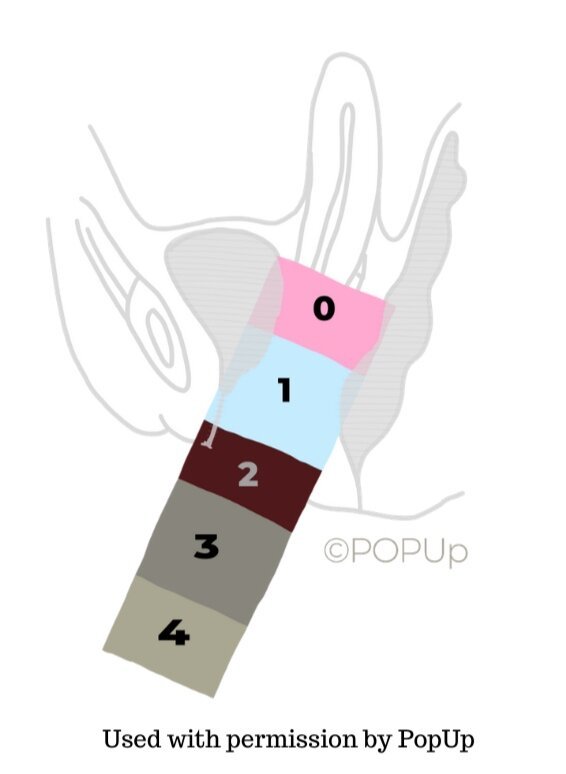
What most women do not know when they are diagnosed with prolapse, is that there are different grades (or severities), based on the extent of the descent of the organ and the woman’s symptoms and level of discomfort.
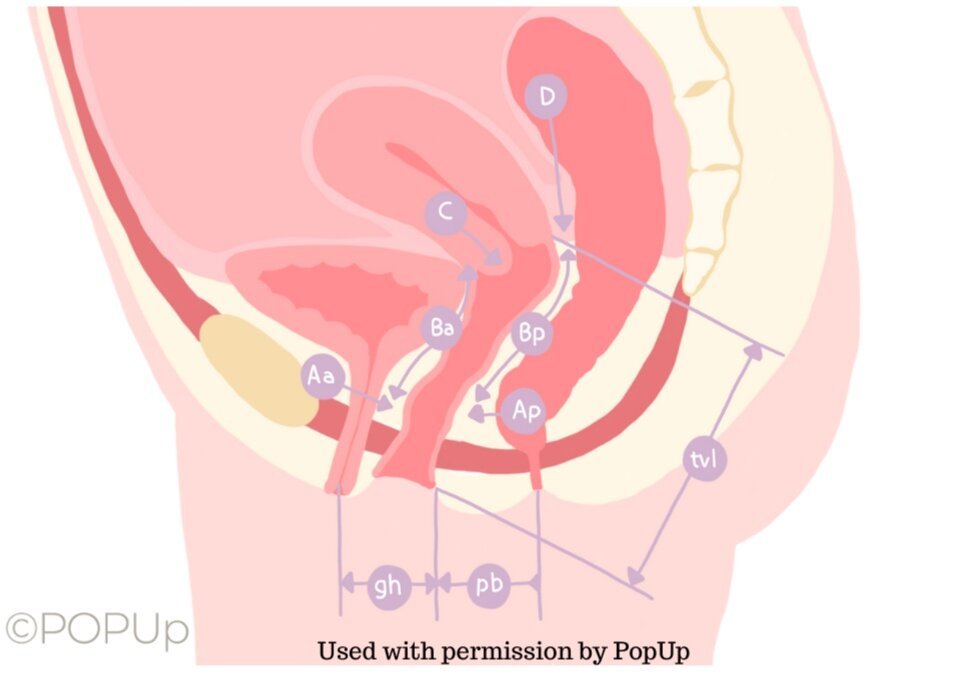
How We Grade or Measure Prolapse
The most commonly used scale to measure a pelvic organ prolapse is called the Baden-Walker Scale (see photo below). Essentially the grade or severity of prolapse increases the lower down the organ is descending with a grade 4 resulting in an organ that is coming significantly outside of the vagina.
OH MY GOSH, This Must Mean I Need Surgery!
Actually, in most cases seeing a pelvic floor physiotherapist can prevent the need for invasive surgeries. In women who choose to undergo surgical repair procedures for pelvic organ prolapse, approximately 50% will experience recurrence (Whiteside et al 2004), (Diane Lee, 2018). This suggests that the underlying reason why the prolapse occurred in the first place was not addressed (poor core strategy, muscular recruitment patterns, poor loading strategies etc). 30% of those who undergo surgery will have a second surgery within 2 years (Salvatore et al 2010).
Although surgery is the right option for some women, it is always recommended to see a pelvic floor physiotherapist and treat the issue conservatively if possible.
Why Pelvic Floor Physiotherapy Can Help
Pelvic organ prolapse can be caused or made worse by a variety of factors, including poor core strategy and weakness, altered movement patterns, pelvic floor muscle weakness (including poor power, poor endurance, poor coordination), constipation and straining. All factors which we can change, strengthen and modify to help eliminate or reduce symptoms!
Your pelvic floor physiotherapist will perform a thorough assessment of your individualized movement patterns, core strategy, pelvic floor muscle strength and the severity of your prolapse. They will design a treatment plan and exercises that target your specific needs with the goal of getting you symptom free, back to the activities you love and prevent the need for invasive surgeries.
Still have questions about pelvic organ prolapse? No problem. Send us an email or give us a call and we would be happy to talk with you.
References:
Diastasis Rectus Abdominis, A Clinical Guide to Those Who are Split Down the Middle. Lee, 2018.
POP UP Pro, 2020.