It is not normal to pee your pants…not even a little bit, not even after childbirth and not even after menopause.
It is not normal to pee your pants…not even a little bit, not even after childbirth and not even after menopause.
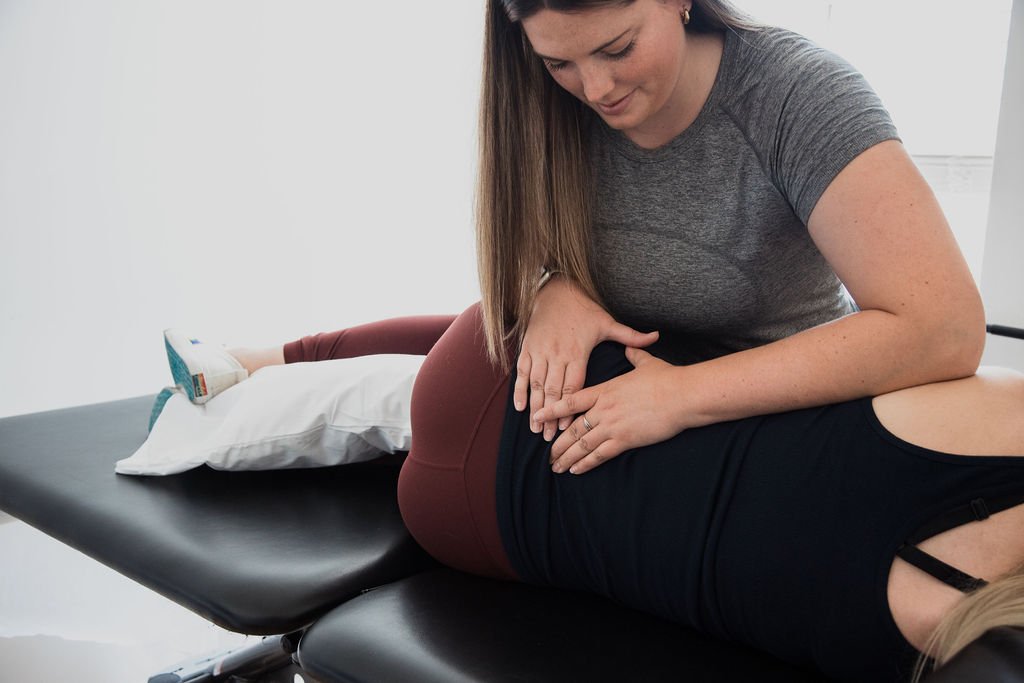
What is Pelvic Health Physiotherapy?
Pelvic health physiotherapy is an evidence-based and specialized field that allows for the assessment and treatment (both external and internally) of common pelvic health disorders such as:
-
Difficulty passing stool, often resulting in straining and bearing down towards the pelvic floor. This chronic straining can cause both weakness and tension in the pelvic floor muscles and can lead to other pelvic floor dysfunctions.
-
Leakage of stool, on its own or with the passing of gas.
-
The involuntary contraction of the muscles around the opening of the vagina that contributes to discomfort, burning and/or pain, resulting in the inability to insert anything (finger, tampon or penis) into the vagina.
-
Chronic pain or discomfort around the opening of the vagina, for which there is no identifiable cause and that occurs for more than 3 months.
Symptoms are often described as a burning, itching or stinging pain or hypersensitivity around the area.
-
A condition in which endometrial-like tissue begins to grow outside of the uterus in the pelvic cavity and can form lesions, cysts and other growths.
Effects 1 in 10 women.
Can be associated with painful intercourse, painful bowel movements, abnormally painful menstrual cycles, cyclical pelvic pain, back or leg pain during menstruation
Please visit: https://endometriosisnetwork.com to learn more
-
IC is defined by the CDC as “A chronic bladder condition resulting in recurring discomfort or pain in the bladder or surrounding pelvic region. People with IC usually have inflamed or irritated bladder walls which can cause scarring or stiffening of the bladder”.
The symptoms of this condition are similar to many pelvic floor dysfunctions and can often be misdiagnosed.
Symptoms typically include: pain that worsens with bladder filling, painful urges to urinate, urinary frequency, night time urination, pain in the pelvis, bladder, urethra or surrounding areas, and painful intercourse.
-
Stress Incontinence: bladder leakage that occurs with an increase in pressure: coughing, sneezing, jumping or liftin.
Urge Incontinence: Bladder leakage that occurs following a strong urge to use the restroom.
Mixed Incontinence: A mixture of both urge and stress incontinence.
-
Pain in these regions can often be due to muscular tension and/or weakness in the pelvic floor or its muscular attachments.
-
A descent of one or more of the pelvic organs into the vaginal canal (most commonly the bladder, uterus or rectum).
It is often associated with feelings of heaviness, pressure or bulging, incomplete emptying of either the bladder or bowel and can cause discomfort with intercourse.
-
The sudden and urgent need to urinate, that may feel almost impossible to postpone.
-
Urinating more than 8 times per day or more than once at night
-
Pain with intercourse can occur in any stage of life, and is never normal.
Pain with sex is often multifactorial but could include, age-related tissue changes, scar tissue dysfunction, and over-active or tense pelvic floor muscles
-
Including birth preparation, postpartum recovery and rehabilitation, exercise prescription and modification, diastasis recti recovery, scar tissue mobilizations and addressing any bowel or bladder issues both prenatally and postnatally. Please see (link to prenatal) and (postpartum page) for more specific information.
Pre-and post surgical rehabilitation for any abdominal or gynecological surgery (hysterectomy, prostatectomy, abdominal surgery).
The strength and function of the pelvic floor and core plays an important role in your recovery and success after surgery.
Do you experience any of the above conditions or symptoms?
Still unsure if you should see a pelvic floor physiotherapist?
Contact us today for a free 15-minute consultation.